Hiatus Hernia
What is it?
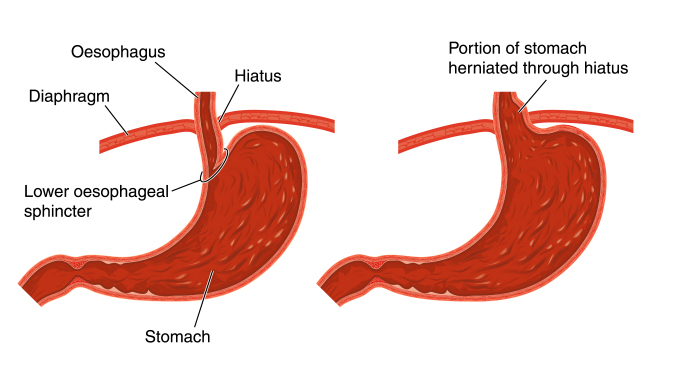 The stomach migrates into the chest through a weakness in the diaphragm. Part or the whole of the stomach can then lie in the chest cavity. Small hiatus hernias are very common and can be found in approximately 50% of individuals over the age of 50.
The stomach migrates into the chest through a weakness in the diaphragm. Part or the whole of the stomach can then lie in the chest cavity. Small hiatus hernias are very common and can be found in approximately 50% of individuals over the age of 50.
Why does it happen?
The diaphragm muscles, which surround the oesophagus, can weaken with time allowing the stomach to push into the chest cavity.
What symptoms do they cause?
Most small hernias will not cause symptoms. When they do, the most common symptom is acid reflux, which is often controlled with simple medication. If surgery is required for reflux then the hernia will be repaired at the same time.
Larger hernias can cause severe reflux and pain. Patients report inability to eat normal sized meals and suffer from regurgitation. The stomach can intermittently rotate or twist resulting in severe pain.
When should I seek help?
Patients with new onset reflux symptoms, pain or difficulty in swallowing should be urgently assessed.
How are they assessed?
 Gastroscopy – is usually the first investigation to be performed for patients presenting with symptoms suggestive of a hiatus hernia.
Gastroscopy – is usually the first investigation to be performed for patients presenting with symptoms suggestive of a hiatus hernia.
Barium Swallow – This is an x-ray test performed whilst drinking contrast. It is painless and quick and gives useful information on the anatomy and size of the hernia.
CT Scan – The CT scan will assess the anatomy of the hernia and give more information about the size of the diaphragmatic defect.
Oesophageal Manometry – is often used to exclude other oesophageal motility disorders such as achalasia.
How should it be managed?
This depends very much on the symptoms. Symptomless hernias should be left alone. If acid reflux is the main problem, then initially lifestyle changes and acid suppression medication maybe successful. For patients with more severe symptoms or a very large hernia, surgery should be considered.
How is the surgery performed?
It is a keyhole procedure. Five small cuts are made in the abdominal wall to allow passage of the instruments. The stomach is brought back down into the abdominal cavity and the diaphragmatic defect is repaired. The procedure normally takes a couple of hours. An anti-reflux procedure is also performed to help prevent post-operative reflux and to help fix the stomach in the abdominal cavity.
More information on Laparoscopic Surgery
How effective is surgery?
Surgery should be very successful and patients report immediate relief of symptoms. The hernias can return, but are usually small and do not cause symptoms. Long-term some patients restart acid suppression medication.
Are there any risks?
Patients can suffer from stomach bloating or increased flatulence. This is due to the inability of air to escape past the new sphincter created to prevent reflux. Avoidance of fizzy drinks and certain foods may improve these symptoms. Temporary difficulty swallowing solid food can occur due to swelling around the oesophagus and stomach resulting from the operation. This resolves over a short period of time and it is rarely an issue long term. Injury to the oesophagus or stomach during the procedure is an uncommon event, which may result in conversion to an open operation.
How long is the recovery period?
Patients are fully mobile after surgery and should commence fluids immediately after surgery. Often, a check contrast study is performed after the procedure before patients start a soft diet. Patients remain on a soft diet for 4 weeks to allow the postoperative swelling to settle.
Patients will often require one or two nights in hospital. This is mainly to build confidence eating and drinking after the surgery. The wound sites will have local anaesthetic injected into them at the time of surgery. This will wear off about 6 hours after the procedure. To stop the sites becoming sore you should take the regular painkillers as instructed. Shoulder tip pain is not uncommon and is due to gas underneath the diaphragm. This should not last longer than 24 hours. You will not be discharged until you are comfortable and eating and drinking. On discharge you should be independent and able to climb a flight of stairs.
Which medications will I require after surgery?
You will be discharged from hospital with a supply of simple painkillers with instructions on how to use them. Regular paracetamol is particularly effective and can be combined with an anti-inflammatory drug (ibuprofen) or a codeine based drug (dihydrocodeine). Anti-inflammatories are not suitable for all patients and should be taken with food. The codeine-based drugs can cause constipation and should be taken with plenty of fluids. Most patients do not require painkillers after 5 days.
When can I return to work?
Generally it is recommended to take two weeks off after surgery. Your ability to return to work will depend on your job and varies between individuals. Patients can often return to work a week after surgery if required. We would not recommend flying immediately after surgery. This should be discussed on a case-by-case basis with the consultant.
When can I drive?
Driving should be avoided in the first week after surgery. Once you can perform an emergency stop in a stationary vehicle and turn to view your blind spot then driving should be safe. It is preferable to contact your insurance company to check for any specific instructions they may have.
Who do I contact if there are concerns?
The group practice telephone is answered in working hours and messages can be left out of hours. Any concerns will be relayed directly to one of the consultant surgeons on receipt. The hospital ward also provides a 24/7 means of contact. They will contact the consultant about any concerns and are able to give advice if required.




